Introduction
Internuclear ophthalmoplegia (INO) is a distinctive ocular motor disorder characterized by impaired horizontal gaze coordination. It results from disruption of the medial longitudinal fasciculus (MLF) which is an essential supranuclear pathway connecting the abducens nucleus of one side with the contralateral oculomotor nucleus. The MLF enables synchronous conjugate eye movements and damage to this fasciculus leads to a failure of adduction of the ipsilateral eye during lateral gaze while the contralateral abducting eye exhibits nystagmus. Convergence is often preserved because it involves separate neural pathways [1].
The etiological spectrum of INO is relatively well defined. Demyelinating disorders including multiple sclerosis (MS) represent the most frequent cause accounting for nearly one-third of all reported cases. These demyelinating lesions tend to involve both sides of the brainstem thereby producing bilateral INO. Another one-third of cases result from ischemic strokes predominantly affecting older patients and usually producing unilateral manifestations. The remaining cases arise from tumors, traumatic brain injury, infections, brainstem hemorrhage and inflammatory lesions [2].
Ischemic INO most commonly originates from small infarcts localized to the dorsal pons where the MLF occupies a relatively extensive portion of the paramedian tegmentum. The midbrain, in contrast, is a rare site for infarct-related INO [3]. Pure isolated INO caused exclusively by midbrain ischemia without associated neurological involvement remains exceptionally uncommon. The paramedian location of the MLF within the midbrain tegmentum means that a very small, precisely placed lesion can selectively disrupt internuclear fibres while sparing neighboring structures. Such focal involvement explains the possibility of an isolated ophthalmoplegic presentation although only limited case reports have described this phenomenon [4].
Because the presenting symptoms of isolated INO may be subtle, patients may report nonspecific complaints such as dizziness, blurred vision or gait instability rather than overt visual diplopia or focal neurological deficits. Without careful ocular and motor evaluation, these cases risk being misinterpreted as peripheral vestibular disorders or benign causes of dizziness potentially delaying diagnosis and appropriate management of posterior circulation stroke [5]. Early neuroimaging, especially diffusion-weighted magnetic resonance imaging (MRI), is crucial for detection of these tiny ischemic lesions affecting the midbrain or pontine tegmentum. Prompt identification not only facilitates initiation of stroke management but also helps prevent future ischemic events and associated disability.
In this context, we report a rare case of pure isolated internuclear ophthalmoplegia resulting from a small focal midbrain infarction. This case highlights diagnostic challenges and clinical significance while adding to the limited existing literature on this uncommon stroke presentation.
Case presentation
A 48-year-old man presented to the emergency department with complaints of sudden-onset dizziness and unsteady gait lasting several hours. There was no history of headache, vomiting, loss of consciousness, seizures, visual blurring, diplopia or facial asymmetry. He denied any preceding trauma or infectious illness. There was no history suggestive of previous neurological disease.
On initial evaluation, the patient was alert and oriented, with a Glasgow Coma Scale score of 15/15. Vital signs were stable, and systemic examination was unremarkable. Cardiovascular and respiratory evaluations revealed no abnormalities.
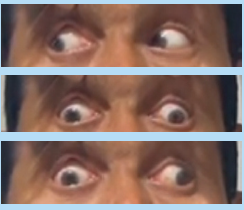
Neurological examination demonstrated intact higher mental functions and normal speech. Cranial nerve assessment showed pupils equal, round and reactive to light. There was no evidence of ptosis or anisocoria. Visual acuity and fundoscopy were normal. Extraocular movement testing revealed a marked abnormality: during attempted left gaze, there was limited adduction of the right eye, while the abducting left eye exhibited multidirectional nystagmus indicating a classical pattern of right-sided internuclear ophthalmoplegia (INO). During right gaze, ocular movements were normal with full adduction of the left eye and no nystagmus in the right eye. Vertical gaze, vestibulo-ocular reflexes, and convergence responses were preserved [Figure 1].
Examination of other cranial nerves showed no deficits. Muscle tone, bulk, and power were normal in all four limbs. Deep tendon reflexes were symmetrical and normal with flexor plantar responses bilaterally. Sensory testing for pain, touch, vibration and proprioception was intact. Finger–nose and heel–shin testing were normal though the patient demonstrated mild gait instability during ambulation. There were no significant cerebellar signs.
Given the ocular findings suggestive of a central brainstem lesion, magnetic resonance imaging (MRI) of the brain was performed. Diffusion-weighted imaging identified a small focal area of acute infarction involving the left lower anterior aspect of the midbrain, anatomically corresponding to the region of the medial longitudinal fasciculus. No additional areas of ischemia were detected.
Based on the clinical features and radiological evidence a diagnosis of isolated right-sided internuclear ophthalmoplegia secondary to focal midbrain ischemic stroke was established. The absence of associated cranial nerve palsies, long-tract signs or cerebellar deficits confirmed this presentation as a rare instance of pure isolated midbrain INO.
Discussion
Mesencephalic infarction is an unusual form of ischemic stroke due to the intricate and redundant arterial supply of the midbrain [6]. In most ischemic cases of internuclear ophthalmoplegia, lesions are localized within the posterior pons where the MLF is relatively larger and more susceptible to small vessel infarctions. Midbrain involvement is seldom isolated and is frequently associated with adjacent oculomotor nerve dysfunction or pyramidal tract involvement [6]. The present patient demonstrated a unique presentation wherein a small focal infarct within the left anterior paramedian midbrain produced pure isolated right INO without additional neurological deficits, emphasizing the selective vulnerability of the MLF at this level.
Similar cases have been documented in the literature and closely parallel our findings. Kim JS et al. reported a patient with unilateral INO caused by a paramedian midbrain infarct detected solely on diffusion-weighted MRI, without associated long-tract deficits or cranial nerve palsies [7]. Musa M et al described an acute presentation of isolated INO secondary to a tiny midbrain ischemic lesion in a clinically stable patient, reinforcing the concept that selective MLF injury may occur with minimal radiological burden [8]. In another report, Haymes et al documented a patient with Midbrain Ischemic Stroke presenting as unilateral INO, which gradually resolved during follow-up [9]. These observations align closely with our case, supporting midbrain ischemia as a rare but well-recognized cause of isolated internuclear ophthalmoplegia.
The diagnostic challenge lies in recognizing INO in patients presenting with vague symptoms such as dizziness or gait instability. Because ocular movement abnormalities may be subtle, incomplete neurological examinations can easily overlook this critical clue. Detailed evaluation of horizontal gaze remains essential, especially in emergency settings where posterior circulation strokes are often under-recognized [10].
Neuroimaging plays a pivotal role in confirming the diagnosis. Small midbrain infarctions may be undetectable on conventional computed tomography scans, making diffusion-weighted MRI indispensable for early and accurate identification. Timely diagnosis allows initiation of appropriate secondary stroke prevention strategies and limits the risk of recurrent ischemic events.
Conclusion
Internuclear ophthalmoplegia can be the sole manifestation of midbrain ischemic stroke. High clinical suspicion, meticulous ocular motor examination, and early neuroimaging are indispensable for identifying posterior circulation infarctions and initiating timely management.
Consent and ethics
Ethics Approval was waived, but confidentiality was ensured, and informed consent was obtained from our case
References
- Virgo JD, Plant GT. Internuclear ophthalmoplegia. Pract Neurol. 2017 Apr;17(2):149-153. doi: 10.1136/practneurol-2016-001428. Epub 2016 Dec 7. PMID: 27927777.
- Hai S, Elkbuli A, Kinslow K, McKenney M, Boneva D. When "looks" can be deceiving - Internuclear ophthalmoplegia after mild traumatic brain injury: Case report and literature review. Int J Surg Case Rep. 2019;63:19-22. doi: 10.1016/j.ijscr.2019.08.032. Epub 2019 Sep 11. PMID: 31539826; PMCID: PMC6796632.
- Breen LA, Hopf HC, Farris BK, Gutmann L. Pupil-sparing oculomotor nerve palsy due to midbrain infarction. Arch Neurol. 1991 Jan;48(1):105-6. doi: 10.1001/archneur.1991.00530130117029. PMID: 1986715.
- Vishwas MS, Whitlow CT, Haq Iu. An unusual aetiology for internuclear ophthalmoplegia. BMJ Case Rep. 2013 Jun 3;2013:bcr2013009290. doi: 10.1136/bcr-2013-009290. PMID: 23737577; PMCID: PMC3702982.
- Nickels C, Keyes C, Astemborski C, Fulton H. The Clue is in the Eyes. A Case Report of Internuclear Ophthalmoplegia. J Educ Teach Emerg Med. 2024 Jan 31;9(1):V1-V8. doi: 10.21980/J8DP9M. PMID: 38344047; PMCID: PMC10854879.
- Shree R, Mahesh KV, Balaini N, Goel A. Oculomotor Cranial Neuropathies: Diagnosis and Management. Ann Indian Acad Neurol. 2022 Oct;25(Suppl 2):S70-S82. doi: 10.4103/aian.aian_167_22. Epub 2022 Jun 8. PMID: 36589037; PMCID: PMC9795710
- Kim JS. Internuclear ophthalmoplegia as an isolated or predominant symptom of brainstem infarction. Neurology. 2004 May 11;62(9):1491-6. doi: 10.1212/01.wnl.0000123093.37069.6d. PMID: 15136670.
- Musa M, Saeed L, Khalil SK, Al-Tikrety NHM, Yousif ZB, Ahmed Y, Almahmood MM, Salman A. Pure Isolated Internuclear Ophthalmoplegia as Presentation of Midbrain Ischemic Stroke: A Case Report. Cureus. 2023 Oct 15;15(10):e47083. doi: 10.7759/cureus.47083. PMID: 38022166; PMCID: PMC10646686.
- Haymes D, Jenson M, Nwachukwu C, Fiester P. Midbrain Ischemic Strokes Presenting as Isolated Internuclear Opthalmoplegia. Cureus. 2021 Sep 8;13(9):e17819. doi: 10.7759/cureus.17819. PMID: 34660029; PMCID: PMC8500245.
- Go S. Posterior Circulation Ischemic Stroke. Mo Med. 2015 May-Jun;112(3):192-6. PMID: 26168589; PMCID: PMC6170115.