Introduction
Plasma cell neoplasms encompass a spectrum of disorders characterized by the clonal proliferation of terminally differentiated B lymphocytes producing monoclonal immunoglobulins [1]. These entities most commonly manifest as multiple myeloma, a systemic disease involving the bone marrow, or less frequently as solitary plasmacytomas. Solitary plasmacytomas are further classified into solitary bone plasmacytoma and extramedullary plasmacytoma (EMP), the latter representing approximately 3–5% of all plasma cell dyscrasias [2]. EMPs arise from soft tissues without evidence of systemic myeloma and most often involve the upper aerodigestive tract, including the nasal cavity, nasopharynx, oropharynx, and paranasal sinuses [3].
Primary involvement of the gastrointestinal tract by extramedullary plasmacytoma is distinctly uncommon, accounting for a small fraction of reported cases, with the stomach and small intestine being the most frequently affected sites. Pancreatic plasmacytoma is exceptionally rare, particularly as a primary lesion, and poses a significant diagnostic challenge due to its nonspecific clinical presentation and radiologic resemblance to more common pancreatic malignancies such as adenocarcinoma, neuroendocrine tumors, or lymphoma [4]. Most pancreatic plasmacytomas described in the literature occur in the setting of known multiple myeloma, whereas isolated primary pancreatic EMPs are limited to sporadic case reports [5].
We describe a primary pancreatic plasmacytoma diagnosed by endoscopic ultrasound (EUS) guided biopsy and immunohistochemistry (IHC) study on the tissue sample.
Case presentation
A 55-year male patient presented with 3 months history of right-sided pain abdomen, breathing difficulty, and pallor. Examination revealed pallor, palpable lump on the right side of the abdomen. Investigations showed hemoglobin of 7.8 gm/dL and the rest are unremarkable. There was a large right-sided heterogeneous mass lesion on abdominal ultrasonography.
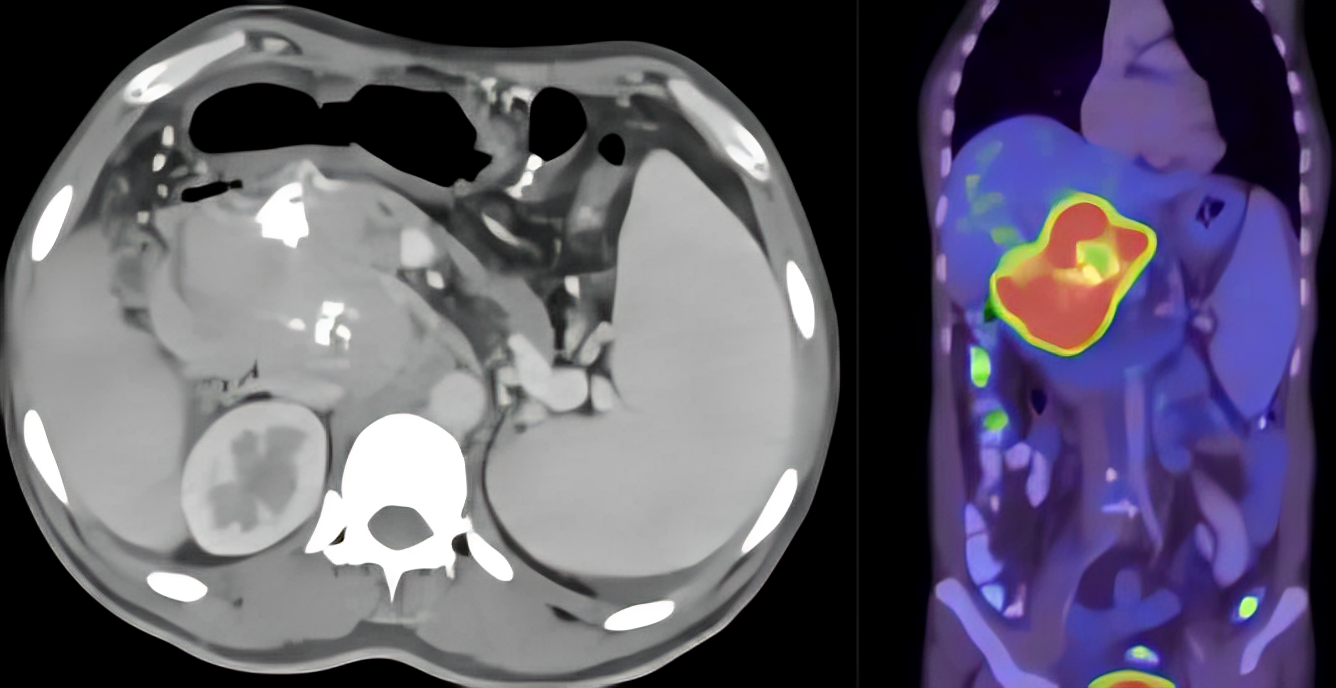
On 18-Fluorodeoxyglucose Positron emission tomography/ computed tomographic (18-FDG-PET/CT) scan, there was a 6.5 X 8.3 X 10.1 cm heterogeneously enhancing lesion with internal calcifications in the head of the pancreas extending into the periportal region, encasing hepatic artery and compressing the portal vein with multiple abdominal collaterals. There was intense FDG tracer uptake with SUV max 10 (Figure 1).
EUS guided biopsy was done using a 22 G needle (Acquire™, Boston Scientific Corporation, Natick MA, USA). Histopathological examination showed sheets of mature and atypical plasmacytoid cells suspicious of plasma cell neoplasm (Figure 2).
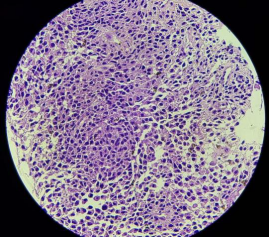
Immunohistochemistry (IHC) showed positivity for Epithelial Membrane Antigen (EMA), CD 138, CD 38, kappa and Multiple Myeloma (MUM) - 1 and negative for cytokeratin, lambda, CD20, CD3, synaptophysin, IgG4, Epstein-Barr encoding region (EBER), chromogranin. All investigations for multiple myeloma were negative including bone marrow aspiration, skeletal survey, serum/urine protein electrophoresis, serum immunofixation. Serum beta2 microglobulin was elevated {3360 ng/ml (700-1800ng/mL)} with altered serum free light chain assay {kappa 149 mg/L;(6.7-22.4); lambda 27.2 mg/L (8.3-27); kappa:lambda ratio 5.48 (0.31-1.56)}, but they were not sufficient enough to make a diagnosis of multiple myeloma. Based on these findings, a diagnosis of extraosseous primary pancreatic plasmacytoma was considered. He received multiple packed red cell transfusions and was referred to an oncologist for external beam radiotherapy.
Discussion
Extramedullary plasmacytoma of the pancreas is very rare (2.3% as per autopsy data). The majority of cases involve the head region (80%) as a solitary mass. Though obstructive jaundice was the most frequent symptom, pancreatitis, gastrointestinal bleeding, and abdominal pain can also occur [6]. Diagnosis is made by FNAC/biopsy commonly obtained under EUS guidance. EUS biopsy of pancreatic masses has high sensitivity and specificity (>95%), thus making it the most frequently used modality to visualize and sample mass lesions in the pancreatic head region. Strong expression of CD 38, CD 56, CD 138, light chain restriction on the tumor tissue will suggest a diagnosis of plasmacytoma [7]. Further diagnostic workup to exclude the presence of plasma cell dyscrasia at other areas in the body must be performed to confirm the presence of primary extramedullary plasmacytoma [8].
Local radiation therapy (40–50 Gy over 4–6 weeks) is the treatment of choice and offers a treatment response in 90–97% cases with a 5-year survival up to 57–61% [9]. Combination chemotherapy including steroids, thalidomide, Bortezomib, vincristine, doxorubicin, etc, and autologous hematopoietic stem cell transplantation offers a good treatment response mainly in those with associated multiple myeloma [7]. Biliary stenting is done for the relief of jaundice [10].
Conclusion
Primary extraosseous plasmacytoma involving the pancreas is very rare. EUS guide biopsy is the best available imaging and sampling modality from pancreatic head mass lesions. Establishing clonality by using IHC and immunophenotyping on the tissue sample should be done. Radiation therapy is the treatment of choice for such pancreatic lesions.
Consent and ethics
Ethics Approval and consent was waived since no identifiable information is published and all patient data was anonymised.
References
- Fend F, Dogan A, Cook JR. Plasma cell neoplasms and related entities—evolution in diagnosis and classification. Virchows Arch. 2023 Jan;482(1):163-177. doi: 10.1007/s00428-022-03431-3.
- Hatipoğlu U, Seyhan M, Ulas T, Dal MS, Altuntaş F. Solitary Plasmacytomas: Current Status in 2025. Hematol Rep. 2025 Jun 30;17(4):32. doi: 10.3390/hematolrep17040032.
- Mogoantă CA, Sarafoleanu C, Osman A, Enache I, Tarabichi S, et al. Extramedullary Plasmacytomas of the Nasal Cavity: Case-Based Perspectives into Optimizing the Diagnostic Differentiation from Inflammatory Polyps. Medicina (Kaunas). 2025 Aug 1;61(8):1406. doi: 10.3390/medicina61081406.
- Lu T, Pu H, Zhao G. Primary pancreatic plasmacytoma: a rare case report. BMC Gastroenterol. 2017 Dec 20;17(1):167. doi: 10.1186/s12876-017-0729-z.
- Rizk RC, Weisberg EM, Fishman EK. Solitary plasmacytoma of the pancreas: A rare case report. Radiol Case Rep. 2024 Feb 17;19(5):1806-1809. doi: 10.1016/j.radcr.2024.01.065.
- Leake PA, Coard KC, Plummer JM. Extramedullary plasmacytoma of the pancreas as an uncommon cause of obstructive jaundice: a case report. J Med Case Rep. 2009 Aug 6;3:8785. doi: 10.4076/1752-1947-3-8785.
- Dass J, Arava S, Mishra PC, Dinda AK, Pati HP. Role of CD138, CD56, and light chain immunohistochemistry in suspected and diagnosed plasma cell myeloma: A prospective study. South Asian J Cancer. 2019 Jan-Mar;8(1):60-64. doi: 10.4103/sajc.sajc_64_17.
- Barbosa P, de Diego C, Anaya J, Busso C, et al. Primary extramedullary plasmacytoma: a rare case presentation. An Bras Dermatol. 2025 Jul-Aug;100(4):501137. doi: 10.1016/j.abd.2025.501137.
- Caers J, Paiva B, Zamagni E, Leleu X, Bladé J, et al. Diagnosis, treatment, and response assessment in solitary plasmacytoma: updated recommendations from a European Expert Panel. J Hematol Oncol. 2018 Jan 16;11(1):10. doi: 10.1186/s13045-017-0549-1.
- Nashed B, Khan A, Issa M, Kohler L, Barawi M. Pancreatic Plasmacytoma: A Case of Recurrent Disease. Cureus. 2022 Jul 1;14(7):e26502. doi: 10.7759/cureus.26502.